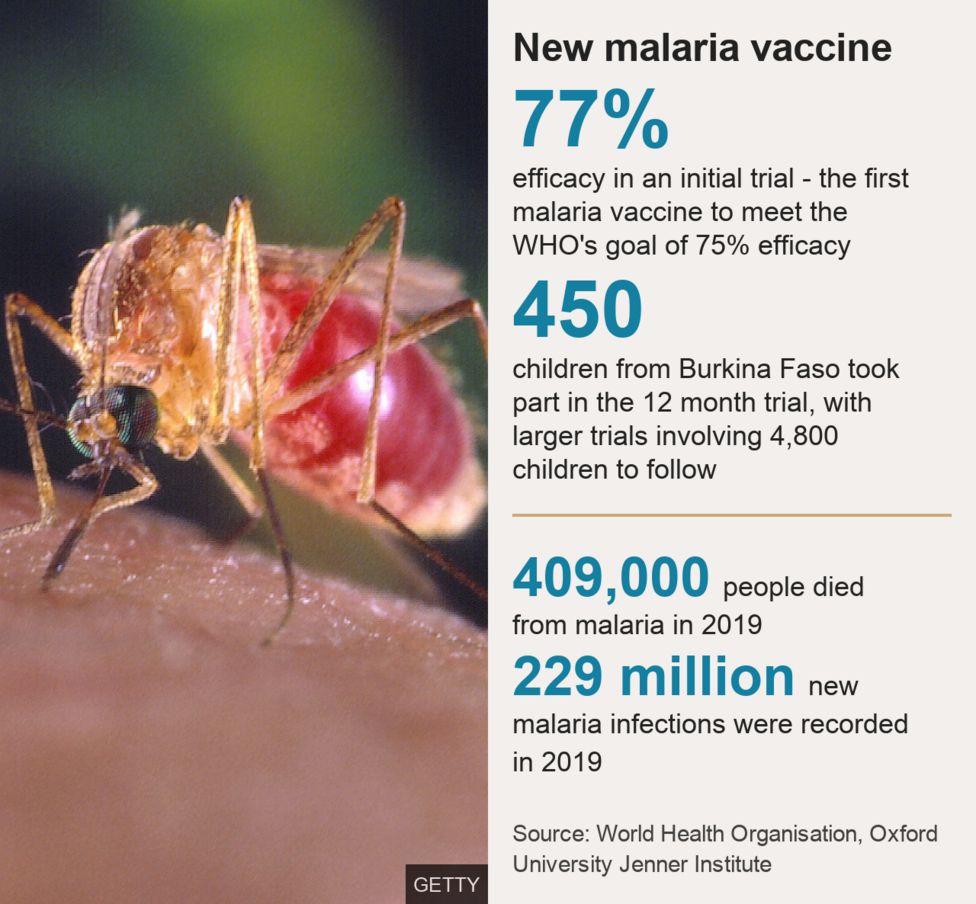
A great year of Malaria research has been overshadowed by the global pandemic of COVID-19. Headlines on promising new vaccines and prevention strategies barely survive the 24-hour news cycle, quickly superseded by the latest COVID-19 related research. Malaria remains a leading cause of death in children under the age of 5 who account for 57% of the > 400,000 deaths/ year from Malaria. With global deaths on this scale, Malaria still very much qualifies as a pandemic but doesn’t get the attention it deserves. Sub-Saharan Africa carries 94% of the burden of disease, a major reason why Malaria has become the neglected pandemic of the poor. The positive results on new vaccines and novel approaches for prevention (monoclonal antibodies) bring much needed hope for eradicating this disease.

A slow ROAD to PROGRESS
It took a year to develop over ten effective vaccines to prevent COVID-19, a disease that did not exist before the end of 2019. Progress on developing a vaccine for Malaria, which has been around for decades, has been very slow. So far Malaria vaccine research have yielded only one partially effective Malaria vaccine (RTS,S or Mosquirix). This vaccine offers a modest 56% protection against Malaria in the first year and effectiveness drops to 36% over 4 years.
Despite its modest effectiveness, Mosquirix has been rolled out as part of ongoing studies in thousands of children in Malawi, Kenya and Ghana. Modeling studies indicate that if Mosquirix use is targeted to areas with the highest malaria burden, it could prevent thousands of childhood deaths. The slow process of developing effective Malaria vaccines is due in part to insufficient funding for Malaria research but also the complex life-cycle of the causal parasite (Plasmodium spp), which is versatile and difficult to target.
New Vaccines, New Hope
This summer a new Malaria vaccine candidate showed promising results in a study in children ages 5-17months. The new vaccine R21 is an updated/modified version of Mosquirix which uses a new adjuvant and generates a stronger immune response. In the phase 2 clinical trial of 450 children in Burkina-Faso, R21 effectively prevented Malaria by up to 77% over a one year period. This level of efficacy meets the preset target of 75% set by the World Health Organization (WHO). A large phase 3 trial will include 4800 children with the hope of confirming these exciting results. The new vaccine is manufactured by the Serum Institute of India, which has pledged to produce 200 million doses of the vaccine every year if it gains approval.
new innovations,NeW CHALLENGES
Another clinical study published this summer used a novel approach , combined a live-parasite vaccine with antimalarial drugs. In this study which included 42 volunteers, the investigators injected participants with sporozoites (the stage of the malaria parasite that is transmitted from the mosquito to humans). They also treated the vaccinated individuals with antimalarial drugs to kill the parasites if they reached the liver or bloodstream so as to prevent the infection of red blood cells and symptomatic malaria. How does this work?- Exposing volunteers to live sporozoites stimulates a protective immune response against future malaria challenge while the antimalarial drug given at the time of vaccination prevents symptomatic malaria from occurring as a result of vaccination.

The volunteers who received the vaccine were infected with malaria 3 months after vaccination to assess the efficacy of the vaccine. 87.5% of those who received the vaccine were protected from Malaria after being exposed to the same malaria strain as the one used in the vaccine. While 77.8% of those infected with a different strain of the parasite were protected. The study is proof of concept that high levels of vaccine efficacy can be achieved with a live-parasite vaccine. It also advances our understanding of what it takes to develop protective immunity to the parasite.
This approach however presents many challenges. Malaria sporozoites cannot be grown in batches in a laboratory for large scale vaccine production and only multiply in the salivary glands of mosquitos. Making enough live-parasite vaccine for larger clinical trials requires isolating sporozoites from millions of mosquitos (through dissection). Also storage of the isolated parasites requires ultra-cold temperatures, which has implications for the vaccine cold chain. These hurdles will increase manufacturing and distribution costs of any potential approved vaccine based on this approach. In addition, the need for combining antimalarial drugs with vaccination could drive development of drug resistance to effective antimalarial drugs. These factors need careful consideration in moving this vaccine forward through larger clinical studies.
Monoclonal Antibodies take on Malaria

Current prophylaxis against Malaria relies almost completely on the use of antimalarial drugs. In a new clinical study led by the National Institutes of Health in the USA, a neutralizing monoclonal antibody (nMAb) was effective in preventing Malaria for up to 9 months in healthy volunteers. nMAbs are laboratory-made proteins, that can attach to harmful pathogens like bacteria, viruses and parasites and target them for destruction by the immune system.
In this study a nMAb called CIS43L3 derived from a naturally occurring neutralizing antibody called CIS43, was delivered through intravenous (IV) infusion or subcutaneous injection to 21 healthy volunteers who had never had Malaria before. CIS43 is an antibody that attaches to a unique site (crucial for facilitating infection), found on all species of malaria sporozoites worldwide. The volunteers were followed for 6 months to assess the safety and tolerability of the intervention and to determine how long CIS43L3 persisted in the blood. The IV infusions and subcutaneous injections of CIS43L3 were safe and well tolerated during the study period with minimal adverse effects.

In the second part of the study, 9 participants who received the nMAb (CIS43L3) treatment and 6 controls (individuals who did not receive nMAbs) were voluntarily exposed to Malaria infection in a controlled setting and closely monitored for symptoms for 21 days. None of the participants treated with nMAbs developed Malaria meanwhile 5/6 individuals in the control group did.
This successful phase I study, supports the viability of monoclonal antibodies for Malaria prevention in travelers visiting endemic regions. It also opens a range of possibilities nMAbs as a prevention tool for controlling seasonal Malaria in Africa and for future elimination campaigns. Ongoing clinical studies will help to better define the role of this exciting new strategy.
Combining old strategies with new ones
Reaching the goal of eliminating Malaria needs more than one intervention. A recent clinical study including 6861 children, showed that combining the Mosquirix vaccine with antimalarial drugs for preventing Malaria provided 72.9% protective efficacy against severe disease and death. The effect of combining two interventions was superior to either intervention alone. Seasonal prevention of Malaria through monthly doses of antimalarial drugs is highly effective in preventing Malaria during high transmission seasons. However, this intervention has been insufficient to reduce the burden of Malaria in the most affected areas. Combining novel vaccines with older interventions could maximize benefits for preventing severe disease and improve on existing interventions for Malaria control.

Breaking the plateau – the final push to eliminating Malaria
In recent years the push to eliminate Malaria hit what felt like an unsurmountable plateau. Effective strategies including; vector control, mosquito nets and chemoprophylaxis prevented millions of deaths but have seen their sustained efficacy wane. Resistance to antimalarial drugs and insecticides is on the rise and population growth in endemic areas has led to more cases. Complacency in the lack of progress means accepting 400,000 plus deaths from Malaria every year, mainly in children. That is what makes the new promising avenues of Malaria research so exciting. Renewed enthusiasm for re-igniting a final push towards eliminating a neglected pandemic and saving lives. At a time when a new pandemic is causing much sadness, I am hopeful for a future without malaria and that is worth celebrating.

Written by Dr. Boghuma K. Titanji




